Cancers are like biological terrorists that hide in the body and then attack it without warning. They can happen in several places, from the lungs to the prostate to the genitalia and essentially anywhere in the body, spreading from its origin to infect other parts rapidly. One of the most talked about types of cancer is breast cancer, something that most of the time affects women but can affect men in a similar but different way. For many years, breast cancer has been researched so that a cure could be developed, but no significant breakthroughs have been made cure-wise.
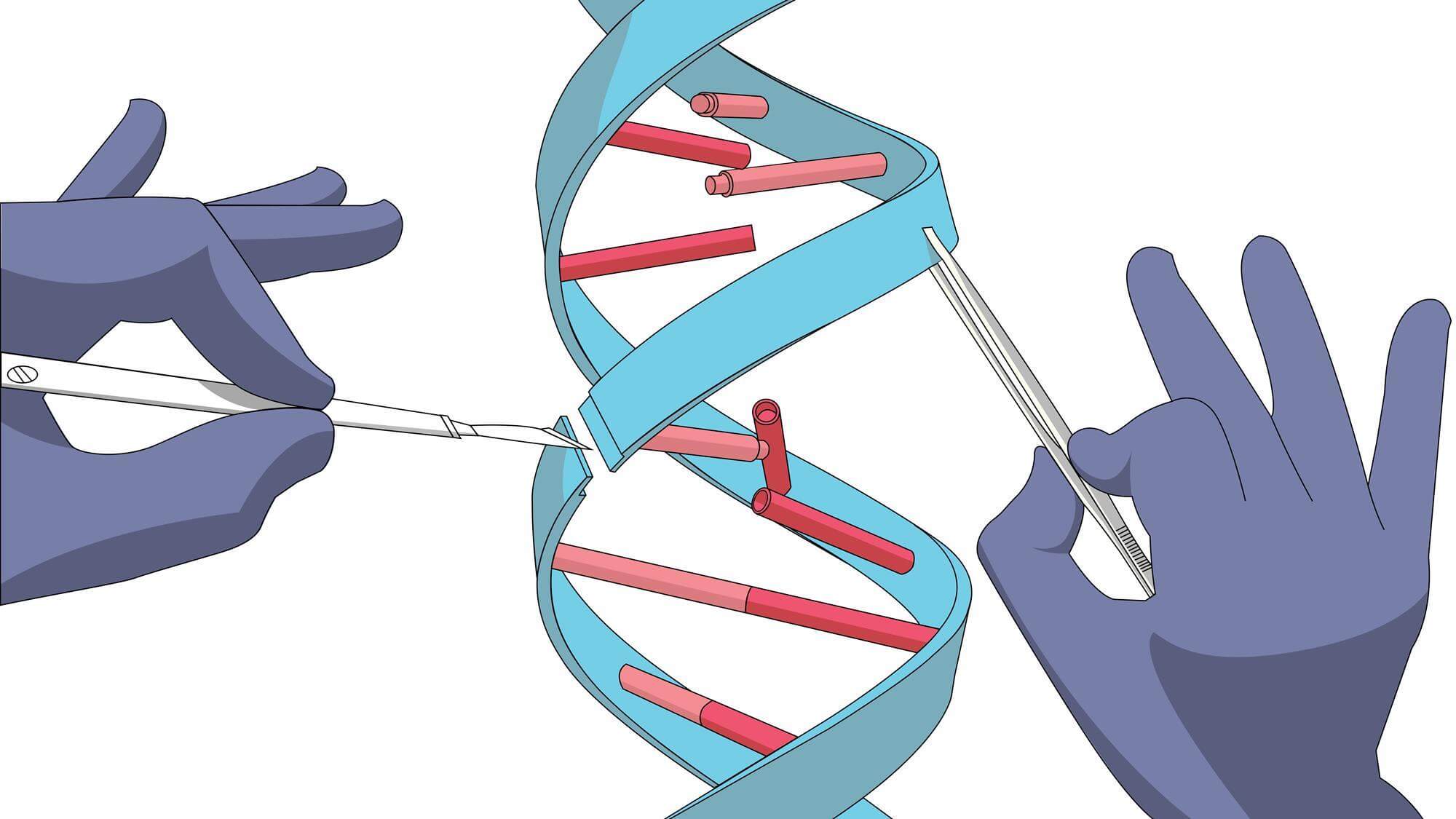
However, a recent study published in
Nature magazine confirms that scientists have an "almost perfect picture of the genetic events that cause breast cancer." It is a "
milestone moment" in genetic history that can shed light on possible treatments and even ways to keep the body from making the cancer cells in the first place. This study, conducted by Cambridge professor Mike Stratton, brought to light all the problems that can occur in body tissues that can cause them to become cancerous, as well as finding 93 genes that can cause cancer in the body if they become mutated in a certain way.
Over the years, drugs have been created to combat certain mutations in genes, but the definite mutations in the body were not known yet, so the treatments were uncertain to be effective all the time in tests. Now that the study has listed what the mutations are specifically, these drugs, like
Herceptin, can be fine tuned and specialized for the mutations that cause cancer. While this seems like a very promising situation, it comes with the stipulation that "60% of the mutations driving cancer are found in just 10 genes," as the article mentions. 10 genes out of the entire human genome is a tricky predicament for scientists, but some of those mutation are so rare that developing drugs for them are not worth it in the first place.
Breast cancer mutations can stem from several different sources, from family to attacking viruses and suffering damage. In the future, as Dr. Serena Nik-Zainal says " In the future, we'd like to be able to profile individual cancer genomes so that we can identify the treatment most likely to be successful for a woman or a man diagnosed with breast cancer." The fact that these mutations have been found in the first place is an important step towards finding the cure for this specific cancer, as well as other ones if the mutations affect genes in similar ways to breast cancer genes. Hopefully in the future, treatments to prevent and cure cancer will be available to the public and harmful chemotherapy will no long have to be the go to option.










/h20-58e655f93df78c5162ea0a1f.jpg)